The UK Health Security Agency launched its latest analysis of the health inequalities in England caused by infectious diseases and environmental health hazards, at the end of April at the Medical Journalists' Association and Health Foundation Symposium 2025 in London.
The Health Inequalities in Health Protection Report, which mainly uses hospital admissions as a measure of infectious disease levels, reveals:
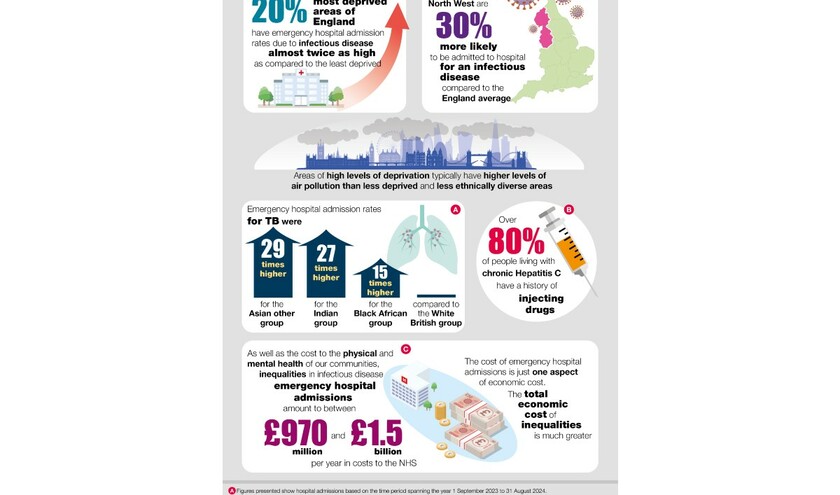
- people living in the 20% most deprived areas in England are almost twice as likely to be admitted to hospital due to infectious diseases than the least deprived
- those living in the North-West are 30% more likely to be hospitalised for an infectious disease (3,600 per 100,000 admissions for Sept 23-Aug 24), compared to the England average (2,800 per 100,000)
- areas of high levels of deprivation typically experience higher levels of air pollution than less deprived and less ethnically diverse areas
- the scale of inequalities between ethnic groups varies by specific disease. For example, emergency admission rates for tuberculosis were 29 times higher for ‘Asian other ‘, 27 times higher for ‘Indian' and 15 times higher for ‘Black African', compared to ‘White British'
- it was estimated that inequalities in emergency infectious disease hospital admissions cost the NHS between £970m and £1.5bn in 2022-23
- it is estimated that infectious diseases were the primary reason for over 20% of hospital bed usage in 2023 to 2024.
In addition, the analysis shows that people living in deprived communities experience higher emergency hospital admission rates, compared to the least deprived communities. The data shows these are:
- twice as high for respiratory diseases in general and up to seven times higher specifically for tuberculosis and six times higher for measles
- twice as high for invasive infections in general, and up to 2.5 times higher specifically for sepsis
- 1.7 times higher for gastrointestinal diseases.
The data shows the people from more deprived areas are also disproportionately impacted by radiation, chemical, climate and environmental hazards through their exposure, direct impact on their health, and the exacerbation of existing health conditions. Areas with high levels of deprivation typically have higher levels of air pollution than less deprived and less ethnically diverse areas.
Dr Leonora Weil, deputy director for health equity and inclusion at UKHSA, said: ‘The report reveals some stark facts on the state of inequalities in health security faced by some people, in particular those living in the most deprived communities and certain areas of the country, some ethnic groups, as well as excluded groups such as those experiencing homelessness.
‘These health protection inequalities - where there are poorer health outcomes based on where you live, your socio-economic status or ethnicity - are avoidable, pervasive, and preventable. That is why it is so important to shine a light on these findings to increase action to support communities to live longer and in better health.'
She added: ‘This data allows us as an organisation, but also with our partners, to then go further to make those differences, to ensure that no community is left behind.
‘Some of the ways that we are doing that is focused and targeted work around vaccine campaigns and vaccine uptake. It's around very specific, tailored and targeted approaches to outbreak response and the pandemic planning that we work towards.
‘It's about partnering, across the health family health organisations at local, regional and national level and internationally, to bring all of that work together, and overall, to ensure that we can unlock the potential in reducing health inequalities.'