The patient safety initiative aims to provide a consistent and understandable way for patients and families to seek an urgent review if their or their loved one's condition deteriorates and they are concerned this is not being responded to.
The scheme is named after Martha Mills, who died from sepsis aged 13 in 2021, having been treated at King's College Hospital, London, due to a failure to escalate her to intensive care and after her family's concerns about her deteriorating condition were not responded to.
Early data from participating hospital sites across England shows that there were at least 573 calls made to escalate concerns about a patient's condition deteriorating in September and October, including from patients, their family, carers and NHS staff.
Around half (286/573) of these calls required a clinical review for acute deterioration, with around one in five (57/286) of the reviews leading to a change in the patient's care – such as receiving potentially life-saving antibiotics, oxygen or other treatment – while remaining on their current wards.
In addition, in the first two months alone, 14 calls made via the new Martha's Rule initiative resulted in a patient needing urgent transfer to ICU.
The NHS is aware of other patients having been moved to High Dependency Units (HDU), coronary care units and other environments, such as returning to operating theatres or radiology, for interventions.
Of the 573 calls in total, 15% were from patients, 76% were from family, carers or designated advocates, and 9% were from NHS staff.
The NHS announced in May 2024 that 143 hospital sites would test and roll out Martha's Rule in its first year as part of the major patient safety initiative.
Professor Sir Stephen Powis, NHS national medical director, said: ‘The introduction of Martha's Rule represents one of the most important changes to patient care in recent years, and we are really encouraged to see the impact it is already having for patients in this first phase.
‘This early data highlights just how essential the Martha's Rule escalation process will be for patients, families and staff, to help ensure those experiencing acute deterioration can be identified and treated at the earliest possible opportunity.'
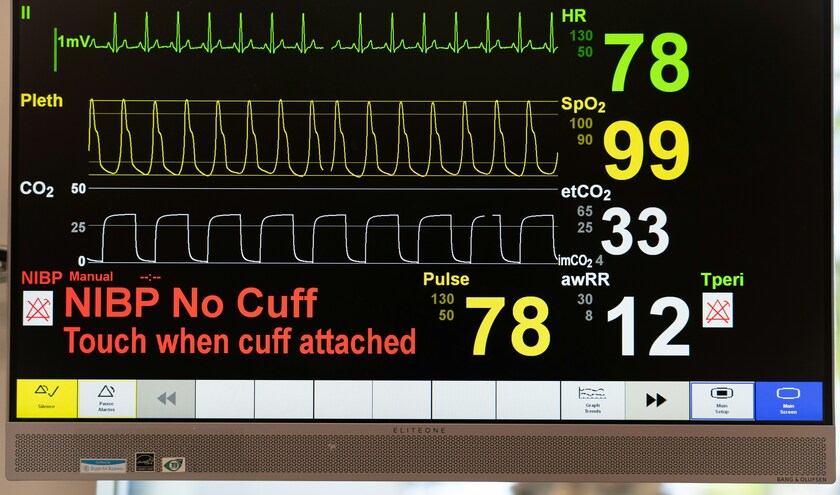
Clinicians at participating hospitals will formally record daily insights and information about a patient's health directly from their families, ensuring any concerning changes in behaviour or condition noticed by the people who know the patient best are considered by staff
The initial target was to enrol at least 100 sites, but due to significant interest from frontline clinicians the programme was expanded, with the first phase of the programme being put in place at 143 locations across the country by March 2025.
Of the 143 hospital sites implementing Martha's Rule in the first year, early data was returned by 136 sites, including 87 sites which have implemented an escalation process for patients and families so far, and 92 sites that have partially or fully implemented an escalation process for staff.
Evaluation of how the system works in these sites over the course of this year will inform proposals for Martha's Rule to be expanded further across all acute hospitals, subject to future government funding.
Health and social care secretary, Wes Streeting, said: ‘The roll-out of Martha's Rule is already playing a role in building a safer NHS by putting patients and their families at the heart of discussions about their healthcare, and early indications are that it could have a transformative impact. This government is committed to making sure every patient is heard.'
Dr Aidan Fowler, NHS national patient safety director and senior responsible officer for the programme, added: ‘Thanks to the engagement and hard work of the 143 pilot sites, we are already seeing life-saving interventions from calls made under Martha's Rule.
‘In addition to providing a valuable failsafe to identify deterioration, this is increasing the sensitivity of our own monitoring as families and staff are very sensitive to changes in patients they know well.'
The introduction of Martha's Rule comes alongside other measures to improve the identification of deterioration, including the rollout last November of a new early warning system for staff treating children. The Paediatric Early Warning System is built on similar processes already in place for adult, newborn, and maternity services.